- Our Products
- Upper Extremity
 AMADEO The hand therapy world champion
AMADEO The hand therapy world champion
Boredom in finger-hand rehabilitation? Not with AMADEO! Motivation in the course of therapy is just as essential as fingers and hands are for daily life. Regardless of whether it is an adult or child, AMADEO increases therapeutic ambition with sophisticated robotics and a playful approach, and also visualizes the smallest successes in all phases of rehabilitation. Bottom line: AMADEO is simply unique. DIEGOBilaterally back to life
DIEGOBilaterally back to life
Finally go fishing again? DIEGO® skilfully assists patients with its unique intelligent weight relief. With its three-dimensional therapeutic area and virtual reality, DIEGO® enables the ideal transfer of what you have learned into everyday life – exactly with the required support. Nothing more and nothing less. TYROSTATION Endless options, well organized
TYROSTATION Endless options, well organized
Anyone who is as versatile as PABLO® and TYMO® needs structure to really unfold. The Tyrostation is home to all individual components of our two all-rounders and also provides perfect ergonomic adaptability for every patient. MYRO Full of variety, versatility, innovation and creativity
MYRO Full of variety, versatility, innovation and creativity
Real objects, power control, touch applications and a whole lot of fun: this is what constitutes goal-oriented, intuitive therapy with MYRO. The sensor-based surface is the basis for creative therapy which brings about meaning and self-determination in daily life. PABLO As versatile as life
PABLO As versatile as life
PABLO® is an all-rounder when it comes to activities of daily living. Position sensors and numerous accessories open up incredibly versatile therapeutic options in a safe environment for patients of all impairment levels.
- Lower Extremity
 PABLO Lower ExtremityPart of PABLO®
PABLO Lower ExtremityPart of PABLO®
Always know where therapy is going
PABLO® Lower Extremity, our gait analysis and training system, precisely measures the parameters which are required for the selection of the most effective therapeutic measures for gait improvement. Simple and location-independent application as well as size-independent measurement makes the package complete – small device, great effect!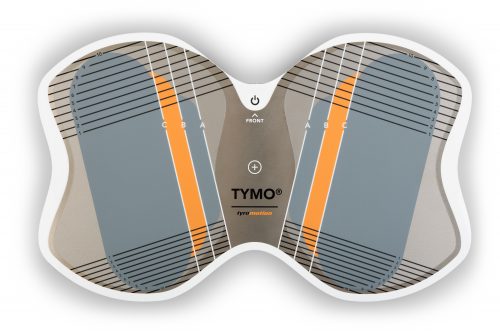 TYMO Balance in perfection
TYMO Balance in perfection
TYMO, a portable posturography system and the world’s thinnest balance platform. Flexible in application, TYMO trains postural control in a sensitive, specific and meaningful manner, and is therefore the basis of all movements. Motivation and fun are included. OMEGO Plus Therapy for all phases of gait rehabilitation gone motivational
OMEGO Plus Therapy for all phases of gait rehabilitation gone motivational
Two separate drives mobilize the patient in an effortless, isolated and focussed manner, and therefore make OMEGO® the long-desired stopgap between mobilization and locomotion. What else remains for patient and therapist to do? Train in a motivated manner, have fun and achieve goals. LEXOGait training at its best
LEXOGait training at its best
Maximum number of steps and intensity, low in height, easy handling and fast setup time: Impossible? It works! With LEXO® patients take the first impressive steps back to mobility and enjoy the feeling that things are finally getting better again.
- MTT-Line
 MTT-Line Medical training therapy
MTT-Line Medical training therapy
The barrier-free MTT-LINE specifically strengthens the six major muscle groups of the human body.
- Software
 TyroS The heart of our technology
TyroS The heart of our technology
Our TyroS software – developed by and together with therapists – is the heart of our technology that combines devices, know-how and therapeutic games. It is a sophisticated therapeutic system that helps challenge and encourage patients.
- Upper Extremity
Health
Stroke – What can I do to help? Information for family members of stroke patients
6. December 2021 ● 4 min. Reading time

Stroke - one Term, many faces
The life of a stroke patient can change from one minute to the next. A stroke can be accompanied by a range of different symptoms:
Weakness or paralysis (hemiparesis/hemiplegia) of one side of the body or individual parts of the body is one of the most common symptoms and often the main one; many times this is what the patient notices first. Suddenly, they may no longer be able to lift their arm or they may fall because their leg won’t support them anymore. These are serious warning signs!
Often, sensation is reduced in one half or individual parts of the body. Other common symptoms include a tingling or unpleasant sensation on the affected side.
The ability to speak and swallow can also be impaired resulting in adaptation to allow for feeding and nutrition. For example, a nasogastric tube could be necessary to feed the patient on a temporary basis or, if permanent assistance is required, a stomach tube may need to be surgically inserted.
Cognitive performance, retentiveness, and memory function can be reduced. The patient’s personality may change as well. Depression is common, as the patient will need time to get used to the physical impairments, limitations, and other changes they are experiencing.
The ability to act and plan might be reduced. Some patients may no longer be able to use daily objects as intended. For example, they may put their undershirt over their shirt.
Another common problem in the period immediately after a stroke is incontinence. Some patients might struggle to retain urine or cannot retain urine at all. Some may require a permanent urinary catheter, because bladder function can remain reduced. Bowel function can also be affected.
Body perception of the affected side can be reduced. Patients may no longer feel stimuli applied to the affected side. In severe cases, the patient might even “neglect” the affected side completely. Some patients even “forget” that the affected side of their body exists.
FAST - How do I recognize a stroke?
FAST is an acronym commonly used to identify if a person is suffering from a stroke; it stands for Face, Arms, Speech and Time.

Face
Ask the person to smile. If that person is having a stroke, one corner of the mouth will droop.
Arms
Ask the person to extend both arms in front of them, palms facing upward. In the case of a stroke, one arm will droop or the palm will turn facedown.
Speech
Ask the person to repeat a simple sentence. The person may not be able to do so or their speech could be slurred.
Time
If the person is unable to complete any of the above tasks, they are in immediate danger. Get help immediately.
Other typical signs of a stroke are a tingling sensation or numbness on one side of the body, severe vertigo, extreme headache, or impaired vision.
The sooner the patient receives medical attention, the better their outlook after the stroke will be.
As a family member of a stroke survivor, what can I do?
Acute phase after a stroke
At the hospital, personal items can make the stay more pleasant. Pictures of family members, flowers, their favorite music or anything else that cheers the patient up can improve the situation. Regular visits, card games or good conversations can also support the healing process.
As a family member can support the patient in this acute phase by the following:
- Address the patient from their affected side and sit on that side when you talk to the patient. This encourages the affected half of the brain to establish new neural connections.
- Speak to the medical staff about using a specific initial touch. For example, lightly touching the patient’s right shoulder before starting a conversation. It alerts the patient to the fact that someone is talking to them. Such an initial touch is commonly used as a support measure for patients with reduced awareness and on intensive care wards especially.
- Close relatives benefit from touching the affected side of the body. Briefly touching the hand can be sufficient. Massaging the hand can also stimulate sensory functions. This stimulus helps the brain to create new connections.
- Take the patient for walks outdoors if that is an option. Nature, natural light and fresh air have a positive impact on mental health.
- Offer support and let the patient know you are there to help.

Rehabilitation after a stroke
For many patients, the hospital stay is immediately followed by a transfer to a rehabilitation institution. The goal is to re-establish as much independence as possible and, if practicable, enable the patient to return to their own home.
Family members can support the patient here as well. Maybe the patient needs some encouragement or diversion, in the form of a walk, or simply your presence. Being ready to listen to the patient can be a big help also.
Many patients realize, during this phase, that their life has changed abruptly. The patient might experience periods of sadness; support from family and friends are even more important now.
Some institutions can coordinate and even encourage family participation in therapies with the patient. If the patient is to be cared for at home with the help of the family, participation and/or training is advisable to gain insight and experience before leaving the medical facility.
What happens after discharge?
Depending on the severity of physical and cognitive limitation, the conditions at home and options for support, a patient may return to his/her own home.
If the stroke patient requires more support with daily tasks, home visits by a nurse can be arranged. If extensive support is needed or safety is a concern, a 24-hour nurse might be a suitable option.
An assisted living facility may allow for a greater degree of independence due to improved accessibility. Those who need continued nursing care and rehabilitation may discharge to a skilled nursing facility (SNF). Patients with the most severe strokes may be transferred to a nursing home.
Outpatient therapy is advisable to maintain the gains made during rehabilitation, to make further progress, and to prevent any secondary damage. Depending on the deficits, physical, occupational, and/or speech therapy, as well as psychological support can be beneficial. If the patient’s mobility makes it impossible to visit a therapist, home visits may be available.
With continued therapy, suitable aids, and adaptation of the patient’s home, a high quality of life may be achieved after a stroke. The support of family and friends will be an important source of assistance and comfort for the patient.
Nevertheless, relatives themselves should also take good care of their health. Only if you are well and healthy, you can watch out for others.
Author: Saskia Wibner
You might also be interested in
4. April 2023
Health
Rehabilitation
Stroke nutrition guidelines for optimal health
Nutrition as the key part in health and well-being of stroke survivors A healthy, balanced …
21. March 2023
Rehabilitation
Kinesio taping in neurology as a useful therapy supplement
The Kinesio tape and its usefulness in neurological therapy What was originally known only from …
7. March 2023
Rehabilitation
Exercises against freezing of gait in Parkinson’s disease
When the legs freeze – how does the symptom “Freezing of Gait” manifest itself? Parkinson’s …








