- Our Products
- Upper Extremity
 AMADEO The hand therapy world champion
AMADEO The hand therapy world champion
Boredom in finger-hand rehabilitation? Not with AMADEO! Motivation in the course of therapy is just as essential as fingers and hands are for daily life. Regardless of whether it is an adult or child, AMADEO increases therapeutic ambition with sophisticated robotics and a playful approach, and also visualizes the smallest successes in all phases of rehabilitation. Bottom line: AMADEO is simply unique. DIEGOBilaterally back to life
DIEGOBilaterally back to life
Finally go fishing again? DIEGO® skilfully assists patients with its unique intelligent weight relief. With its three-dimensional therapeutic area and virtual reality, DIEGO® enables the ideal transfer of what you have learned into everyday life – exactly with the required support. Nothing more and nothing less. TYROSTATION Endless options, well organized
TYROSTATION Endless options, well organized
Anyone who is as versatile as PABLO® and TYMO® needs structure to really unfold. The Tyrostation is home to all individual components of our two all-rounders and also provides perfect ergonomic adaptability for every patient. MYRO Full of variety, versatility, innovation and creativity
MYRO Full of variety, versatility, innovation and creativity
Real objects, power control, touch applications and a whole lot of fun: this is what constitutes goal-oriented, intuitive therapy with MYRO. The sensor-based surface is the basis for creative therapy which brings about meaning and self-determination in daily life. PABLO As versatile as life
PABLO As versatile as life
PABLO® is an all-rounder when it comes to activities of daily living. Position sensors and numerous accessories open up incredibly versatile therapeutic options in a safe environment for patients of all impairment levels.
- Lower Extremity
 PABLO Lower ExtremityPart of PABLO®
PABLO Lower ExtremityPart of PABLO®
Always know where therapy is going
PABLO® Lower Extremity, our gait analysis and training system, precisely measures the parameters which are required for the selection of the most effective therapeutic measures for gait improvement. Simple and location-independent application as well as size-independent measurement makes the package complete – small device, great effect! TYMO Balance in perfection
TYMO Balance in perfection
TYMO, a portable posturography system and the world’s thinnest balance platform. Flexible in application, TYMO trains postural control in a sensitive, specific and meaningful manner, and is therefore the basis of all movements. Motivation and fun are included. OMEGO Plus Therapy for all phases of gait rehabilitation gone motivational
OMEGO Plus Therapy for all phases of gait rehabilitation gone motivational
Two separate drives mobilize the patient in an effortless, isolated and focussed manner, and therefore make OMEGO® the long-desired stopgap between mobilization and locomotion. What else remains for patient and therapist to do? Train in a motivated manner, have fun and achieve goals. LEXOGait training at its best
LEXOGait training at its best
Maximum number of steps and intensity, low in height, easy handling and fast setup time: Impossible? It works! With LEXO® patients take the first impressive steps back to mobility and enjoy the feeling that things are finally getting better again.
- MTT-Line
 MTT-Line Medical training therapy
MTT-Line Medical training therapy
The barrier-free MTT-LINE specifically strengthens the six major muscle groups of the human body.
- Software
 TyroS The heart of our technology
TyroS The heart of our technology
Our TyroS software – developed by and together with therapists – is the heart of our technology that combines devices, know-how and therapeutic games. It is a sophisticated therapeutic system that helps challenge and encourage patients.
- Upper Extremity
Rehabilitation in Pandemics is an integral component of a comprehensive management
In some cases, the pandemic led to a reduction of rehabilitation services due to cancellation of elective surgeries, reallocation of resources to critical items such as personal protective equipment and intensive care unit equipment, as well as the redistribution of staff.
However, patients recovering from COVID-19 need rehabilitation and many facilities are now seeing an increased demand for services. Providers are challenged to satisfy the rehabilitation needs for large numbers of patients while ensuring high standards of care, maintaining social distancing and other restrictions.
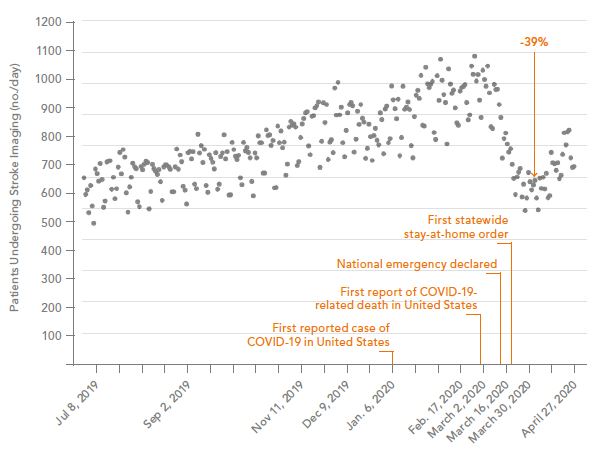
Massive Drop in Stroke Evaluations
A study titled Collateral Effects of COVID-19 on Stroke, published May 8, 2020 in the New England Journal of Medicine, showed that the number of people evaluated for acute stroke in the U.S. has dropped by 39% during COVID-19.1
This health emergency and the resulting adaptation of healthcare facilities has also influenced the rehabilitation treatments of non-COVID-19 pathologies. Early rehabilitation is strongly correlated with optimal clinical and functional recovery and the delay of post-stroke rehabilitation is related to poor functional recovery.1
During a pandemic, immediate care for people who experience a stroke is of critical importance to allow access to treatments and effectively reduce death and disability.
Stroke in COVID-19 Patients under 50
Five cases of large-vessel stroke in patients younger than 50 years were reported from New York in the New England Journal of Medicine. All five patients tested positive for Covid-19. Two of the patients delayed calling an ambulance because they were concerned about going to a hospital during the pandemic.2
Awareness seems advisable that social distancing, isolation, and reluctance to present to the hospital may contribute to poor outcomes after stroke.
Post Intensive Care Syndrome (PICS)
There are grounds for concern that a significant number of people will emerge from intensive care with Post Intensive Care Syndrome (PICS) and that being on a ventilator battling through COVID-19 in intensive care for more than a week may result in disability.3
During a stay in the intensive care unit (ICU) the most common form of physical impairment acquired is neuromuscular weakness, with more than 25% of individuals having poor mobility, recurrent falls, or paresis.4
A study in survivors of severe critical illness shows that early physical and occupational therapy during critical illness are the best evidence-based target interventions for reducing the long-term physical complications.4
Recent experience from Italy already reveals that especially patients with serious COVID-19 illness need a tailored neuromotor and respiratory rehabilitation program.5
“Early rehabilitation of the COVID-19
patients can enhance pulmonary,
respiratory function, reduce complications,
improve function, cognitive impairments
and quality of life.” 6
Optimizing outcomes
Rehabilitation may reduce complications associated with admission to an ICU, such as post intensive care syndrome (PICS); it aims to optimize a patient’s recovery and reduce the extent of disability. Rehabilitation interventions can help to address many consequences of severe COVID-19, including physical, cognitive, and swallowing impairments, and provide psychosocial support. Older patients, and those with pre-existing health conditions, may be more vulnerable to the effects of severe illness, and rehabilitation can be particularly beneficial for maintaining their prior levels of independence.6
Rehabilitation improves the health outcomes of patients with severe cases of COVID-19 and benefits health services through.7
By using powerful novel technologies in rehabilitation such as robotics, sensor technology, virtual reality and gamification, Tyromotion makes it possible to guide patients through the rehabilitation process with more motivation, increased intensity and dosage of therapies.
Rehabilitation technology and robotics can help with individually tailored and highly intensive therapy as well as with providing therapy to more patients.8,9
“As in any disaster, the role of
medical rehabilitation in pandemics
is an integral component of
comprehensive management.”6
OMEGO® Plus may help with rehab during COVID-19 by sup-porting early rehabilitation & a comprehensive therapy pro-gram within one device.
- Reduce number of times a patient moves between diffe-rent devices.
- OMEGO® Plus addresses endurance, strength and coordi-nation all in one device.
- Disinfection once per session and not after every device.
- Software guided goal-oriented therapy sequences can reduce the number of physical interactions between pa-tients and therapists.
- Multiple OMEGO®’s can be safely spaced apart and allow the treatment of several patients at once by a single therapist. This facilitates continuous indirect supervision of all patients with minimal direct contact.
|
|
This is why we believe OMEGO® Plus can help on the pathway to recovery during a pandemic. |
References
1 Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral Effect of Covid-19 on Stroke Evaluation in the United States. N Engl J Med. 2020 May 8.
2 Oxley TJ, Mocco J, Majidi S, et al. COVID-19 Cases. Large-Vessel Stroke as a Presenting Feature of Covid-19 in the Young. N Eng J Med. 2020 May 13.
3 https://www.rehabpub.com/conditions/fear-of-post-intensive-care-syndrome/? campaign_type=newsletter
4 Fan E, Dowdy DW, Colantouni E, et al. Physical Complications in Acute Lung Injury Survivors: A 2-Year Longitudinal Prospective Study. Crit Care Med. 2014;42(4):849–859.
5 Brugliera L, Spina A, Paola Castellazzi P, et al. Department of Rehabilitation and Functional Recovery, I.R.C.C.S. San Raffaele Scientific Institute, Vita-Salute University, Milan. Rehabilitation of COVID-19 patients. J Rehabil Med 2020; 52:4.
6 Khan F, Amatya B. Medical Rehabilitation in Pandemics: Towards a new perspective. J Rehabil Med. 2020 Apr 9.
7 Pan American Health Organization (PAHO). Rehabilitation considerations during the COVID-19 outbreak. 2020.
8 Aprile I, Germanotta M, Cruciani A, Loreti S, Pecchioli C, Cecchi F, Montesano A, Galeri S, Diverio M, Falsini C, Speranza G, Langone E, Papadopoulou D, Padua L, Carozza M. Upper Limb Robotic Rehabilitation after Stroke: A Multicenter, Randomized Clinical Trial. J Neurol Phys Ther. 2020 Jan; 44(1): 3-14.
9 Calabrò RS, Accorinti M, Porcari B, Carioti L, Ciatto L, Billeri L, Andronaco VA, Galletti F, Filoni S, Naro A. Does hand robotic rehabilitation improve motor function by rebalancing interhemispheric connectivity after chronic stroke? Encouraging data from a randomised-clinical-trial. Clin Neurophysiol. 2019 May; 130(5):767-780.









