- Our Products
- Upper Extremity
 Amadeo Finger-Hand-Rehabilitation
Amadeo Finger-Hand-Rehabilitation
Amadeo is giving hands back their grip and fingers their finesse. Patients who are barely able or unable to grasp can perform hundreds of robot-assisted grasping movements. It won’t train a new Mozart. But it will help patients return to the piano, handwriting Christmas cards, and grabbing life firmly by the horns. DiegoShoulder-Arm-Rehabiliation
DiegoShoulder-Arm-Rehabiliation
Diego is designed to strengthen what’s important. Whether proximal or distal training, Diego purposefully supports the rehabilitation of natural motion, allows the handling of everyday objects to be relearned, and is usable by adults and children alike. Myro Interactive and task-specific therapy
Myro Interactive and task-specific therapy
Myro is made for making humans get better! The sensor-based surface enables task-oriented rehabilitation with real objects, trains the patient’s cognitive abilities, and improves motor abilities of the upper extremity. Pablo Upper Extremity Rehabilitation
Pablo Upper Extremity Rehabilitation
As a multifunctional rehabilitation device with comprehensive accessories, Pablo enhances classical therapy exercises with biofeedback, objective assessments, and gamification. It won´t train the next Picasso. But it will help patients to take back control of their lives. Tyrostation The perfect therapy setting
Tyrostation The perfect therapy setting
The Tyrostation is home to all components of Pablo and Tymo and provides ergonomic adaptability for patients. Sometimes, it´s about the little things in life – or therapy.
- Lower Extremity
 LexoGait and Locomotion
LexoGait and Locomotion
Lexo is a revolutionary gait trainer and impresses with fast setup, high patient activity and optimal trunk support. It encourages active participation and enables therapists to focus fully on their patients. Omego Plus Gait training for the goals across all phases
Omego Plus Gait training for the goals across all phases
More than just a therapy bike! Omego Plus combines uni- and bilateral leg training, leg press, stepper, cycling & foot lift training in one device. Stride stronger with Omego Plus!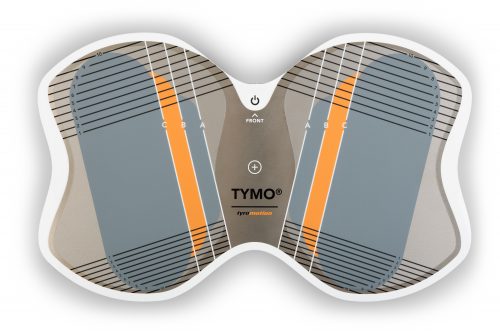 Tymo Balance training and postural control
Tymo Balance training and postural control
Small but powerful! Tymo is a versatile measurement and therapy system for the whole body. In addition to the standing position, Tymo offers a wide range of options for maximum variety during therapy.
- MTT-Line
 MTT-LineMedical training therapy
MTT-LineMedical training therapy
Get back in the game with the MTT-Line! The Medical Training Therapy devices are specifically designed to strengthen the six major muscle groups of the human body. Barrier free and maximum adjustability make the devices accessible for all types of patients.
- Software
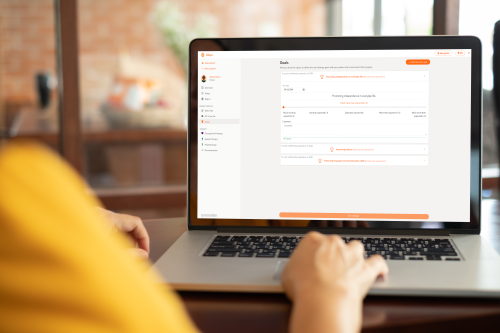 Maya Therapy Platform
Maya Therapy Platform
Maya reduces paperwork, standardizes documentation, and automates reporting, making administration effortless and efficient. Designed for therapists to work wonders!
- Upper Extremity
Health
Stroke – What can I do to help? Information for family members of stroke patients
6. December 2021 ● 4 min. Reading time

Stroke - one Term, many faces
The life of a stroke patient can change from one minute to the next. A stroke can be accompanied by a range of different symptoms:
Weakness or paralysis (hemiparesis/hemiplegia) of one side of the body or individual parts of the body is one of the most common symptoms and often the main one; many times this is what the patient notices first. Suddenly, they may no longer be able to lift their arm or they may fall because their leg won’t support them anymore. These are serious warning signs!
Often, sensation is reduced in one half or individual parts of the body. Other common symptoms include a tingling or unpleasant sensation on the affected side.
The ability to speak and swallow can also be impaired resulting in adaptation to allow for feeding and nutrition. For example, a nasogastric tube could be necessary to feed the patient on a temporary basis or, if permanent assistance is required, a stomach tube may need to be surgically inserted.
Cognitive performance, retentiveness, and memory function can be reduced. The patient’s personality may change as well. Depression is common, as the patient will need time to get used to the physical impairments, limitations, and other changes they are experiencing.
The ability to act and plan might be reduced. Some patients may no longer be able to use daily objects as intended. For example, they may put their undershirt over their shirt.
Another common problem in the period immediately after a stroke is incontinence. Some patients might struggle to retain urine or cannot retain urine at all. Some may require a permanent urinary catheter, because bladder function can remain reduced. Bowel function can also be affected.
Body perception of the affected side can be reduced. Patients may no longer feel stimuli applied to the affected side. In severe cases, the patient might even “neglect” the affected side completely. Some patients even “forget” that the affected side of their body exists.
FAST - How do I recognize a stroke?
FAST is an acronym commonly used to identify if a person is suffering from a stroke; it stands for Face, Arms, Speech and Time.

Face
Ask the person to smile. If that person is having a stroke, one corner of the mouth will droop.
Arms
Ask the person to extend both arms in front of them, palms facing upward. In the case of a stroke, one arm will droop or the palm will turn facedown.
Speech
Ask the person to repeat a simple sentence. The person may not be able to do so or their speech could be slurred.
Time
If the person is unable to complete any of the above tasks, they are in immediate danger. Get help immediately.
Other typical signs of a stroke are a tingling sensation or numbness on one side of the body, severe vertigo, extreme headache, or impaired vision.
The sooner the patient receives medical attention, the better their outlook after the stroke will be.
As a family member of a stroke survivor, what can I do?
Acute phase after a stroke
At the hospital, personal items can make the stay more pleasant. Pictures of family members, flowers, their favorite music or anything else that cheers the patient up can improve the situation. Regular visits, card games or good conversations can also support the healing process.
As a family member can support the patient in this acute phase by the following:
- Address the patient from their affected side and sit on that side when you talk to the patient. This encourages the affected half of the brain to establish new neural connections.
- Speak to the medical staff about using a specific initial touch. For example, lightly touching the patient’s right shoulder before starting a conversation. It alerts the patient to the fact that someone is talking to them. Such an initial touch is commonly used as a support measure for patients with reduced awareness and on intensive care wards especially.
- Close relatives benefit from touching the affected side of the body. Briefly touching the hand can be sufficient. Massaging the hand can also stimulate sensory functions. This stimulus helps the brain to create new connections.
- Take the patient for walks outdoors if that is an option. Nature, natural light and fresh air have a positive impact on mental health.
- Offer support and let the patient know you are there to help.

Rehabilitation after a stroke
For many patients, the hospital stay is immediately followed by a transfer to a rehabilitation institution. The goal is to re-establish as much independence as possible and, if practicable, enable the patient to return to their own home.
Family members can support the patient here as well. Maybe the patient needs some encouragement or diversion, in the form of a walk, or simply your presence. Being ready to listen to the patient can be a big help also.
Many patients realize, during this phase, that their life has changed abruptly. The patient might experience periods of sadness; support from family and friends are even more important now.
Some institutions can coordinate and even encourage family participation in therapies with the patient. If the patient is to be cared for at home with the help of the family, participation and/or training is advisable to gain insight and experience before leaving the medical facility.
What happens after discharge?
Depending on the severity of physical and cognitive limitation, the conditions at home and options for support, a patient may return to his/her own home.
If the stroke patient requires more support with daily tasks, home visits by a nurse can be arranged. If extensive support is needed or safety is a concern, a 24-hour nurse might be a suitable option.
An assisted living facility may allow for a greater degree of independence due to improved accessibility. Those who need continued nursing care and rehabilitation may discharge to a skilled nursing facility (SNF). Patients with the most severe strokes may be transferred to a nursing home.
Outpatient therapy is advisable to maintain the gains made during rehabilitation, to make further progress, and to prevent any secondary damage. Depending on the deficits, physical, occupational, and/or speech therapy, as well as psychological support can be beneficial. If the patient’s mobility makes it impossible to visit a therapist, home visits may be available.
With continued therapy, suitable aids, and adaptation of the patient’s home, a high quality of life may be achieved after a stroke. The support of family and friends will be an important source of assistance and comfort for the patient.
Nevertheless, relatives themselves should also take good care of their health. Only if you are well and healthy, you can watch out for others.
Author: Saskia Wibner
You might also be interested in
4. April 2023
Health
Rehabilitation
Stroke nutrition guidelines for optimal health
Nutrition as the key part in health and well-being of stroke survivors A healthy, balanced …
21. March 2023
Rehabilitation
Kinesio taping in neurology as a useful therapy supplement
The Kinesio tape and its usefulness in neurological therapy What was originally known only from …
7. March 2023
Rehabilitation
Exercises against freezing of gait in Parkinson’s disease
When the legs freeze – how does the symptom “Freezing of Gait” manifest itself? Parkinson’s …



 Contact
Contact 

 Contact
Contact