- Our Products
- Upper Extremity
 Amadeo Finger-Hand-Rehabilitation
Amadeo Finger-Hand-Rehabilitation
Amadeo is giving hands back their grip and fingers their finesse. Patients who are barely able or unable to grasp can perform hundreds of robot-assisted grasping movements. It won’t train a new Mozart. But it will help patients return to the piano, handwriting Christmas cards, and grabbing life firmly by the horns. DiegoShoulder-Arm-Rehabiliation
DiegoShoulder-Arm-Rehabiliation
Diego is designed to strengthen what’s important. Whether proximal or distal training, Diego purposefully supports the rehabilitation of natural motion, allows the handling of everyday objects to be relearned, and is usable by adults and children alike. Myro Interactive and task-specific therapy
Myro Interactive and task-specific therapy
Myro is made for making humans get better! The sensor-based surface enables task-oriented rehabilitation with real objects, trains the patient’s cognitive abilities, and improves motor abilities of the upper extremity. Pablo Upper Extremity Rehabilitation
Pablo Upper Extremity Rehabilitation
As a multifunctional rehabilitation device with comprehensive accessories, Pablo enhances classical therapy exercises with biofeedback, objective assessments, and gamification. It won´t train the next Picasso. But it will help patients to take back control of their lives. Tyrostation The perfect therapy setting
Tyrostation The perfect therapy setting
The Tyrostation is home to all components of Pablo and Tymo and provides ergonomic adaptability for patients. Sometimes, it´s about the little things in life – or therapy.
- Lower Extremity
 LexoGait and Locomotion
LexoGait and Locomotion
Lexo is a revolutionary gait trainer and impresses with fast setup, high patient activity and optimal trunk support. It encourages active participation and enables therapists to focus fully on their patients. Omego Plus Gait training for the goals across all phases
Omego Plus Gait training for the goals across all phases
More than just a therapy bike! Omego Plus combines uni- and bilateral leg training, leg press, stepper, cycling & foot lift training in one device. Stride stronger with Omego Plus!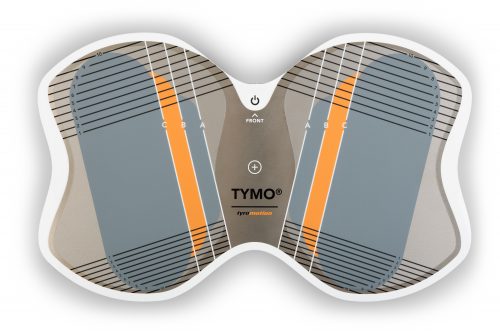 Tymo Balance training and postural control
Tymo Balance training and postural control
Small but powerful! Tymo is a versatile measurement and therapy system for the whole body. In addition to the standing position, Tymo offers a wide range of options for maximum variety during therapy.
- MTT-Line
 MTT-LineMedical training therapy
MTT-LineMedical training therapy
Get back in the game with the MTT-Line! The Medical Training Therapy devices are specifically designed to strengthen the six major muscle groups of the human body. Barrier free and maximum adjustability make the devices accessible for all types of patients.
- Software
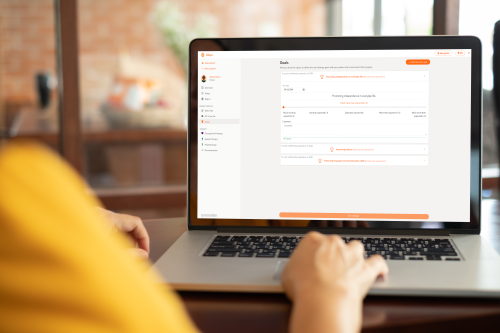 Maya Therapy Platform
Maya Therapy Platform
Maya reduces paperwork, standardizes documentation, and automates reporting, making administration effortless and efficient. Designed for therapists to work wonders!
- Upper Extremity
Rehabilitation
Exercises against freezing of gait in Parkinson’s disease
Hannes Aftenberger ●
7. March 2023 ● 6 minutes
When the legs freeze – the motor symptom “Freezing of Gait”
If you are a person affected by it, you may already know: You walk around your home and want to turn into another room. Suddenly, however, nothing works at all. The steps become smaller and smaller, you finally come to a complete standstill and suddenly can’t move even an inch forward. Some patients also describe that although they are still able to take small steps in place, they still cannot move from the spot. A feeling of being frozen occurs. This state can last for different lengths of time – from a few minutes up to half an hour or even longer.
Most often, this symptom occurs when affected persons start walking (like a kind of start inhibition at the gait initiation), make turns, pass through narrow passages like doors, carry out dual tasks (like talking while walking), or try to reach a specific destination. In the literature, this symptom is called “Freezing of Gait (FOG)” and, along with postural instability, is one of the most noticeable signs of Parkinson’s disease.
Management of FOG through attention training and other exercises
Patients, therapists, and studies include and describe various exercises and methods to influence freezing of gait. These include directing your attention to your walking. Even if the symptom is not yet noticeable, you should consciously draw attention to your own steps. This can delay, or ideally even prevent, FOG.
If FOG has already set in, there are also measures and options to counteract freezing at the moment of immobility. There are also exercises that, if done regularly, can gradually reduce the frequency of freezing attacks.
Attention during walking
It all starts with introspection – perhaps the critical locations in the house are already known, or there are familiar paths where FOG tends to occur? Many patients also report certain times of day when FOG is more likely to occur, or they have been able to identify a correlation with their medication regimen. All of these things – once they are known – can improve FOG management and better prepare you for FOG each time.
If you feel that you are about to experience a freezing episode and may have difficulty walking, try to take larger and more rhythmic steps and try to lift your knees higher than normal. Especially when turning in a different direction, make sure that the steps are executed very specifically. By attentively and consciously setting each step, FOG can thus be reduced.
Regular gait training
Patients with Parkinson’s disease report – and there is also strong evidence in the literature – that gait training can positively influence FOG. We would like to present some of these suggestions and show you how you can use them to design your training and to improve your gait pattern.
Define a specific walking distance and try walking it in different ways:
Variant 1: Take large steps forward and then backward.
Variant 2: When walking, make sure the track is evenly spaced.
Variant 3: Walk and raise knees high with each step.
Variant 4: Take large sideways steps in both directions.
You can increase the influence of the exercises by also ensuring your arms move evenly while walking; that is, the arms swing back and forth in opposite directions – similar to two pendulums.
Tips for gait training
- During gait training, make sure to be in a safe environment. Before you start, make sure everything is out of the way so there is no risk of falling or injury.
- Don’t strain yourself. First, choose a distance that you can easily manage that won’t leave you out of breath. With time and practice, you can gradually increase the walking distance. If necessary, you can also use aids such as walking sticks for your own safety.
- If you have little space in your home, remember that you can also walk in circles while performing the exercises. In any case, the gait/walk should remain rhythmic and smooth.
- Don’t be afraid to ask your therapist for support as well. He or she can work with you to develop a personalized gait training program that is completely tailored to your individual needs.

There are several gait training options that have proven successful in the management of freezing.
“Cueing”- giving a clear impulse
“Cueing” refers to an impulse that helps to stay in gait rhythm or to break free from the feeling of being “frozen in place.” This stimulus can be not only auditory or visual, but also tactile. It can be set either by yourself or with the use of various tools.
Auditory cueing
Set an impulse in the above exercises by…
… counting along loudly and rhythmically.
… singing a rhythmic song.
Make use of various tools for auditory cueing. You can put on headphones and have the song or rhythm played to you. Try different versions and methods and find out whether it is more effective for you to count by yourself or to use headphones to help you. Some patients even manage to free themselves from the immobility that has already set in by counting out loud.
Visual cueing
In addition to acoustic stimuli, there is also visual cueing, in which a visual stimulus is given. In practice, it looks like this:
Variant 1: Select and define distances on your walking route that you want to reach.
Variant 2: Depending on the possibility, lines can be marked on the floor with the help of adhesive tape, across which you want to step each time.
Variant 3: Another option is special adaptations you can put on your walking sticks that project a laser strip in front of your feet on the floor, across which you want to step. It is best to ask your therapist, who can help you obtain one.
Tactile cueing
Tactile cueing involves a touch stimulus in the form of a light rhythmic tap on the thighs while walking – this can positively influence the flow of movement. There are also devices that can be attached to the legs that prompt walking via a vibration pulse.

Practicing and training in a group not only brings more fun and motivation, but mutual exchange about Parkinson’s is promoted.
Group therapy
Training alone at home can become monotonous over time. Find a suitable group where you can practice with others and motivate each other. Check with your therapist, look for support groups, or research the Internet to see if group gait training is available in your area.
Studies have shown that freezing in particular – when trained in a group – can be positively influenced. By the way, this also includes regular dancing to counteract freezing.
Treadmill training
Treadmill training also has several benefits for patients with Parkinson’s disease. You are independent of wind and weather and can therefore train regularly. While swinging your arms during walking is recommended, the handrails allow you to practice in a safe way, as you can hold on to them at any time. There is a wide range of treadmill models for home use. However, those who don’t want to invest in a home treadmill, can alternatively use one as part of a gym subscription or exercise therapy. Research has shown that regular treadmill training can counteract freezing. This type of exercise seems to have a positive effect after just a few weeks. But here, too, you should first seek advice from an expert: The treating therapist will be happy to explain the correct operation and appropriate settings of the device to you.

By training on the treadmill, positive effects on Freezing of Gait could be observed - and this was seen after just a few weeks.
A diagnosis of Parkinson’s disease and the symptoms that accompany it can often severely limit patients’ lives. However, proper exercises and a regular exercise routine can help regain confidence and self-determination in everyday life, thus improving quality of life.
Literature:
DGNR – Deutsche Gesellschaft für Neurorehabilitation e.V. (n.d.). 2017, from http://www.dgnr.de/
Ginis, P., Nackaerts, E., Nieuwboer, A., & Heremans, E. (2018). Cueing for people with Parkinson’s disease with freezing of gait: A narrative review of the state-of-theart and novel perspectives. Annals of Physical and Rehabilitation Medicine, 61(6), 407–413.
Gómez-González, J., Martín-Cashttps://doi.org/10.1016/j.rehab.2017.08.002as, P., & Cano-de-la-Cuerda, R. (2019). Effects of auditory cues on gait initiation and turning in patients with Parkinson’s disease. Neurología (English Edition), 34(6), 396–407.
Nieuwboer, A., Kwakkel, G., Rochester, L., Jones, D., van Wegen, E., Willems, A. M., Chavret, F., Hetherington, V., Baker, K., & Lim, I. (2007). Cueing training in the home improves gait-related mobility in Parkinson’s disease: The RESCUE trial. Journal of Neurology, Neurosurgery & Psychiatry, 78(2), 134–140.
You might also be interested in
4. April 2023
Health
Rehabilitation
Stroke nutrition guidelines for optimal health
Nutrition as the key part in health and well-being of stroke survivors A healthy, balanced …
21. March 2023
Rehabilitation
Kinesio taping in neurology as a useful therapy supplement
The Kinesio tape and its usefulness in neurological therapy What was originally known only from …
7. March 2023
Rehabilitation
Exercises against freezing of gait in Parkinson’s disease
When the legs freeze – how does the symptom “Freezing of Gait” manifest itself? Parkinson’s …



 Contact
Contact 


 Contact
Contact