- Our Products
- Upper Extremity
 Amadeo Finger-Hand-Rehabilitation
Amadeo Finger-Hand-Rehabilitation
Amadeo is giving hands back their grip and fingers their finesse. Patients who are barely able or unable to grasp can perform hundreds of robot-assisted grasping movements. It won’t train a new Mozart. But it will help patients return to the piano, handwriting Christmas cards, and grabbing life firmly by the horns. DiegoShoulder-Arm-Rehabiliation
DiegoShoulder-Arm-Rehabiliation
Diego is designed to strengthen what’s important. Whether proximal or distal training, Diego purposefully supports the rehabilitation of natural motion, allows the handling of everyday objects to be relearned, and is usable by adults and children alike. Myro Interactive and task-specific therapy
Myro Interactive and task-specific therapy
Myro is made for making humans get better! The sensor-based surface enables task-oriented rehabilitation with real objects, trains the patient’s cognitive abilities, and improves motor abilities of the upper extremity. Pablo Upper Extremity Rehabilitation
Pablo Upper Extremity Rehabilitation
As a multifunctional rehabilitation device with comprehensive accessories, Pablo enhances classical therapy exercises with biofeedback, objective assessments, and gamification. It won´t train the next Picasso. But it will help patients to take back control of their lives. Tyrostation The perfect therapy setting
Tyrostation The perfect therapy setting
The Tyrostation is home to all components of Pablo and Tymo and provides ergonomic adaptability for patients. Sometimes, it´s about the little things in life – or therapy.
- Lower Extremity
 LexoGait and Locomotion
LexoGait and Locomotion
Lexo is a revolutionary gait trainer and impresses with fast setup, high patient activity and optimal trunk support. It encourages active participation and enables therapists to focus fully on their patients. Omego Plus Gait training for the goals across all phases
Omego Plus Gait training for the goals across all phases
More than just a therapy bike! Omego Plus combines uni- and bilateral leg training, leg press, stepper, cycling & foot lift training in one device. Stride stronger with Omego Plus!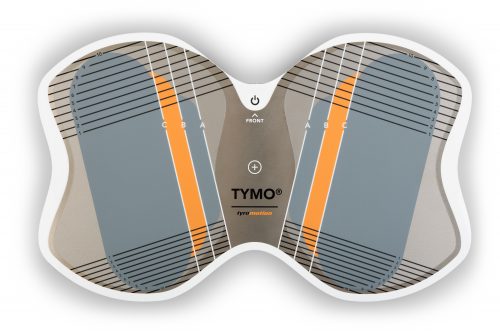 Tymo Balance training and postural control
Tymo Balance training and postural control
Small but powerful! Tymo is a versatile measurement and therapy system for the whole body. In addition to the standing position, Tymo offers a wide range of options for maximum variety during therapy.
- MTT-Line
 MTT-LineMedical training therapy
MTT-LineMedical training therapy
Get back in the game with the MTT-Line! The Medical Training Therapy devices are specifically designed to strengthen the six major muscle groups of the human body. Barrier free and maximum adjustability make the devices accessible for all types of patients.
- Software
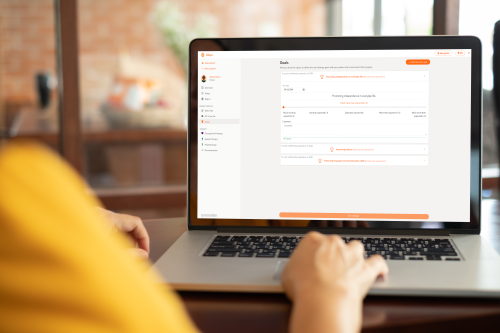 Maya Therapy Platform
Maya Therapy Platform
Maya reduces paperwork, standardizes documentation, and automates reporting, making administration effortless and efficient. Designed for therapists to work wonders!
- Upper Extremity
Health
Parkinson’s disease symptoms – Between stiffness and shaking
4. July 2022 ● 5 minutes

Parkinson's disease is often accompanied by the symptom of shaky hands - which is why it is colloquially known as shaking palsy.
The development of Parkinson’s disease – what happens in the body?
When suffering from idiopathic Parkinson’s (without discernible cause), the dopamine-producing nerve cells in the mesencephalon (substantia nigra) slowly die. The reason for this is still unknown. The falling dopamine level in the brain results in impaired communication between nerve cells and an imbalance of neurotransmitters. The body can compensate for this deficiency sufficiently for quite some time so that it goes unnoticed by the patient. The first typical symptoms occur once approximately 60 % of dopamine-producing nerve cells have died. It is hypothesized that this causes the shaking (tremor) that is so typical for Parkinson’s disease.
Nonspecific early symptoms of Parkinson’s disease
Even years before apparent symptoms appear, there may be unspecific symptoms indicating Parkinson’s:
- Changes in dream phases: Usually, the body is limp while we dream, almost as if paralyzed. It has been shown that years before Parkinson’s was diagnosed, patients would actually perform the actions they dreamt of (talking, laughing, gesturing).
- Sense of smell might be reduced or disappears completely.
- Inexplicable joint pain, especially in the arms
- Interference with color perception
- Change in handwriting: The longer the patient writes, the smaller and more illegible the writing becomes.
- Depression, fatigue, exhaustion
- Unspecific digestive issues

Some symptoms, such as joint pain in the arms, may occur years before PD is diagnosed.
The most common symptoms of Parkinson’s disease
Slowness of movements (bradykinesia):
The patient’s movements become slower and the range of motion decreases (hypokinesia), which may worsen to total loss of motion (akinesia). Both voluntary and autonomic muscle control may be affected. All movements are unnaturally slow. The posture is stooped, steps are small, and/or patients scuttle or shuffle when they walk. Starting or stopping a movement is also difficult. Sudden stopping of a movement, so-called “freezing“, occurs frequently. This increases the risk of falling. Facial expressions and gestures are reduced; laughing and crying seem delayed and look like a grimace. The face seems to become an unmoving mask. The abilities to speak and swallow may also be affected. Fine motor function worsens: manipulating buttons or opening/closing zippers becomes difficult; writing becomes illegible; brushing teeth becomes impossible.
Reactions and accompanying movements are also affected. The patient doesn’t move his or her arms when walking or simply “falls” into a seat due to poor balance. Parkinson’s disease also reduces the speed of thought processes.
Stiff muscles:
Parkinson’s disease increases muscle tone, causing the body to become stiffer. Both contracting and stretching muscles may be affected. Deliberate relaxation is not possible. Passively moving parts of the body results in the so-called “cogwheel” phenomenon. The muscles relax in bursts, like a cogwheel. Typical for this stiffness of the muscles is the “floating pillow” sign. When the patient lies down on their back, they cannot put their head down. The muscles are so tense that the head seems to “float” above the pillow.
Shaking (tremor):
When relaxed, arms or legs may shake. One half of the body is often more severely affected than the other. Shaking usually occurs in the hands and arms.
Insufficient stability of posture (postural control):
Righting and postural reflexes are continuously and unconsciously correcting the position and posture of our body. This balancing process prevents falls. In patients with Parkinson’s disease, the righting and postural reflexes are interrupted. Patients struggle to remain upright. Sudden, unforeseen changes in movement can no longer be countered and corrected in time. Their gait becomes insecure, and they tend to fall more often.
Other symptoms:
Patients may also have difficulties swallowing or suffer from incontinence, insomnia, depression, and dementia. Hallucinations, delusions, and paranoia often accompany dementia.
Does Parkinson’s start in the intestines?
It is becoming more evident that the nervous system in the abdomen is closely linked to the brain. Animal studies were able to show that incorrectly shaped proteins (alpha-synucleins) form in the digestive tract and can spread along the vagus nerve into the brain. Whether Parkinson’s actually starts in the digestive tract and the consequences for treatment options remain open at this time.
How is Parkinson’s disease diagnosed?
Parkinson’s disease is often diagnosed based on its typical symptoms. The severity of the disease is assessed based on the Hoehn and Yahr Scale, amongst others. It records the disruption of movements. The Unified Parkinson’s Disease Rating Scale (UPDRS) is another standardized tool for recording clinical symptoms.
Physicians and therapists may perform additional active and passive movement tests to get a clearer picture of the disease presentation and progression:
- Quick movements like screwing in a lightbulb are no longer possible (dysdiadochokinesis).
- Passive movement, such as of the elbow joint, results in the cogwheel phenomenon, i.e. the relaxation of muscles in short bursts.
- Tests to check balance and posture stability are also performed (Berg Balance Scale, Timed Up and Go Test).
Imaging technology such as CT or MRI can be used to exclude other diseases with similar symptoms.
If Parkinson’s is suspected but not confirmed, specific medication can be used to clarify the diagnosis. If the symptoms improve with medication, the patient likely has Parkinson’s. If no change is observed, there may be other causes for the Parkinson’s-like symptoms (secondary or atypical Parkinson’s syndrome).
Therapy options for Parkinson’s disease
Treatment for Parkinson’s disease must be tailored to the individual patient. Good success can be achieved with medication, physiotherapy, occupational therapy, speech therapy, and psychological support.
Medication
The goal of medication is to reduce the lack of dopamine in the brain. The neurotransmitter is either administered directly as medication or the breakdown of existing dopamine is inhibited. The active agents used depends mainly on the age of the patient. The goal of medication is symptom reduction.
Deep Brain Stimulation, DBS
If certain conditions are met, deep brain stimulation may be the method of choice for treating the symptoms of Parkinson’s. In a surgical procedure, small electrodes are implanted into certain areas of the brain. The so-called “leads” generate electrical impulses that control abnormal brain activity.
Non-medication based treatment
Physiotherapy, occupational therapy, speech therapy, and psychological support are essential parts of treating Parkinson’s. Interdisciplinary cooperation of different therapeutic and medical disciplines can considerably alleviate symptoms.Physiotherapy knows several techniques to improve agility, balance, coordination, strength, and endurance. Technology-based therapy equipment can supplement other treatments.
When living with Parkinson’s disease, independent practice, continued participation in daily life, and support through therapeutic aids can improve the quality of life of patients. The goal is to maintain the independence of the patient in everyday situations for as long as possible.

Good to know
Every year on April 11, World Parkinson’s Day takes place.
The aim of World Parkinson’s Day is to create greater awareness of this disease and the living situation of those affected and their relatives.
Sources:
Physiotherapy in Parkinson’s Disease: A Meta-Analysis of Present Treatment Modalities, 2020
In vivo distribution of α-synuclein in multiple tissues and biofluids in Parkinson disease, 2020
Deep Brain Stimulation in Parkinson’s Disease, 2019
Initiation of Parkinson’s disease from gut to brain by δ-secretase, 2019
You might also be interested in
4. April 2023
Health
Rehabilitation
Stroke nutrition guidelines for optimal health
Nutrition as the key part in health and well-being of stroke survivors A healthy, balanced …
21. March 2023
Rehabilitation
Kinesio taping in neurology as a useful therapy supplement
The Kinesio tape and its usefulness in neurological therapy What was originally known only from …
7. March 2023
Rehabilitation
Exercises against freezing of gait in Parkinson’s disease
When the legs freeze – how does the symptom “Freezing of Gait” manifest itself? Parkinson’s …



 Contact
Contact 

 Contact
Contact