- Our Products
- Upper Extremity
 Amadeo Finger-Hand-Rehabilitation
Amadeo Finger-Hand-Rehabilitation
Amadeo is giving hands back their grip and fingers their finesse. Patients who are barely able or unable to grasp can perform hundreds of robot-assisted grasping movements. It won’t train a new Mozart. But it will help patients return to the piano, handwriting Christmas cards, and grabbing life firmly by the horns. DiegoShoulder-Arm-Rehabiliation
DiegoShoulder-Arm-Rehabiliation
Diego is designed to strengthen what’s important. Whether proximal or distal training, Diego purposefully supports the rehabilitation of natural motion, allows the handling of everyday objects to be relearned, and is usable by adults and children alike. Myro Interactive and task-specific therapy
Myro Interactive and task-specific therapy
Myro is made for making humans get better! The sensor-based surface enables task-oriented rehabilitation with real objects, trains the patient’s cognitive abilities, and improves motor abilities of the upper extremity. Pablo Upper Extremity Rehabilitation
Pablo Upper Extremity Rehabilitation
As a multifunctional rehabilitation device with comprehensive accessories, Pablo enhances classical therapy exercises with biofeedback, objective assessments, and gamification. It won´t train the next Picasso. But it will help patients to take back control of their lives. Tyrostation The perfect therapy setting
Tyrostation The perfect therapy setting
The Tyrostation is home to all components of Pablo and Tymo and provides ergonomic adaptability for patients. Sometimes, it´s about the little things in life – or therapy.
- Lower Extremity
 LexoGait and Locomotion
LexoGait and Locomotion
Lexo is a revolutionary gait trainer and impresses with fast setup, high patient activity and optimal trunk support. It encourages active participation and enables therapists to focus fully on their patients. Omego Plus Gait training for the goals across all phases
Omego Plus Gait training for the goals across all phases
More than just a therapy bike! Omego Plus combines uni- and bilateral leg training, leg press, stepper, cycling & foot lift training in one device. Stride stronger with Omego Plus!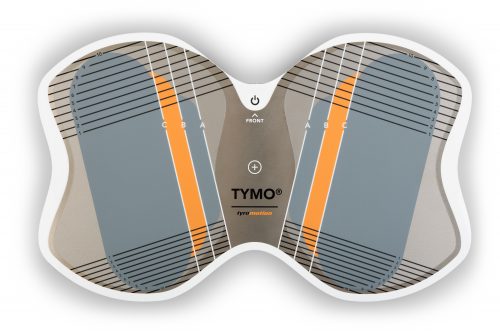 Tymo Balance training and postural control
Tymo Balance training and postural control
Small but powerful! Tymo is a versatile measurement and therapy system for the whole body. In addition to the standing position, Tymo offers a wide range of options for maximum variety during therapy.
- MTT-Line
 MTT-LineMedical training therapy
MTT-LineMedical training therapy
Get back in the game with the MTT-Line! The Medical Training Therapy devices are specifically designed to strengthen the six major muscle groups of the human body. Barrier free and maximum adjustability make the devices accessible for all types of patients.
- Software
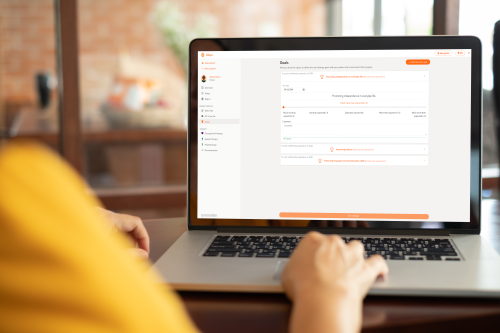 Maya Therapy Platform
Maya Therapy Platform
Maya reduces paperwork, standardizes documentation, and automates reporting, making administration effortless and efficient. Designed for therapists to work wonders!
- Upper Extremity
Health
Multiple Sclerosis – How the autoimmune disease turns life upside down
11. April 2022 ● 6 min. Reading Time

Causes of MS
MS is a chronic inflammatory autoimmune disease. The immune system attacks the body’s own cells in the patient’s brain and spinal cord.
Despite worldwide research, the causes of MS are not yet clear. Classical MS theory assumes that three factors cause the condition to manifest:
- Genetic predisposition: Approximately 15% of MS patients have immediate or extended family members who were also diagnosed with MS
- Environmental influences in childhood: Viral infections (e.g. Epstein-Barr virus) or vitamin D deficiency
- Trigger event in adulthood: It is not yet absolutely clear what such a trigger event might be. In most cases, emotional stress precedes the first acute episode of the disease.
There is a consensus in the scientific community that complex interactions of environmental, genetic, and epigenetic factors are the probable cause for onset of the disease.
What are the symptoms of MS?
The symptoms are varied and manifest differently in each patient. This is why MS is also called the “disease of a thousand faces”.
There are different types of MS. In most cases (85-90%), the disease is intermittent-relapsing.
The neurological symptoms appear relatively suddenly, subside over the course of several weeks, and often regress completely.
MS is not always diagnosed immediately. A diagnosis could take years.
As the disease progresses, the symptoms may not regress completely after the acute episode and residual symptoms remain. It is possible that the condition becomes chronic and symptoms may worsen gradually over time.
In rare cases, the disease progresses from the onset (10-15%). This form knows no clear, separate acute episodes.
The symptoms are varied and depend on the areas of the brain and/or spinal cord where inflammatory lesions occur. Some of the possible symptoms are listed below:
- Optic neuritis (inflammation of the optic nerve) Common first symptom – Deterioration of vision; usually occurs in one eye only; foggy/hazy vision; pain may occur
- Paresthesia Common first symptom – Sensory impairments such as tingling, tightness around the joints; often symmetrical, often described as feeling sock-like or glove-like; difficulties with determining temperature (hot/cold); numbness
- Ocular motility disorder – e.g.: double vision; nystagmus (uncontrolled horizontal or vertical eye movements)
- Paresis (weakness) / plegia (paralysis) – Patients often report initial mild weakness, such as a “tiredness” in the arm/leg; frequent twisting of the ankle, or joint stiffness; Paralysis rarely occurs in the early stages.
- Problems with coordination – Often develop during the course of the disease; e.g. episodes of rotary vertigo, loss of balance, tremors
- Vegetative dysfunction – Change in bladder function (e.g. frequent urges to urinate; frequent urinary tract infections); sexual dysfunction; increased or decreased sweating
- Psychophysical symptoms – Fatigue (abnormal fatigability) – marked exhaustion/fatigue that improves with rest
- Psychological changes – Cognitive impairment: e.g. reduced attention or cognitive performance; depression
MS has many faces:
- Appoximately1/3 of patients with MS experience no significant impairment throughout their life.
- Approximately 1/3 of patients with MS experience limitations that interfere with everyday activities. Living a normal life is mostly possible (e.g.: professional occupation, family planning).
- Approximately 1/3 of patients with MS experience significant impairments (e.g.: inability to work, loss of ability to walk).
How is MS diagnosed?
Preparing a detailed medical history and good patient documentation are critical for diagnosing MS.
If MS is suspected, the suspicion can be verified by taking a sample of cerebrospinal fluid from the spinal canal or with the help of an MRI.
Drug therapy for MS
During an acute episode, cortisone therapy can help to shorten the episode and reduce its consequences.
Options for long-term therapy depend on the form of MS. Various medications are used to influence the immune system. The immune system is either suppressed (immunosuppression) or influenced (immunomodulation). An effective immunotherapy can have a significant positive impact on the progression of the disease or the impairment caused by it.
Rehabilitation and conservative MS therapy
Rehabilitation for MS patients is designed to help preserve physical, social, and/or occupational skills. The treatment options are as varied as the symptoms of the condition itself. Physical and occupational therapy, speech therapy and psychotherapy can help patients to cope with everyday activities.

Rehabilitation goals:
- Preserving or improving functional capabilities
- Promoting independence and mobility
- Promoting and maintaining involvement in family life, social environment, and work
- Preventing and/or treating possible deficits caused by MS
- Alleviating psychological changes
- Reducing the amount of care required
An essential part of outpatient therapy is an active lifestyle – whenever possible. Studies show that physiotherapy increases patient mobility and muscle strength, reduces fatigue, and improves the quality of life.

Living with MS
Accepting the diagnosis and learning to develop strategies for new daily routines will help patients keep control and maximize independence.
Deliberate “disease-free” time spent with friends, outdoors, or engaging in a hobby can help individuals to see themselves as persons rather than patients. However, this may be easier said than done. Conversations with other patients (e.g. in self-help groups) or psychotherapy may be helpful.
Physical activity, in particular, is important for maintaining skills and physical awareness. Nevertheless, it is also important to accept one’s own limits. Too little, but also too much activity can have an adverse effect on the progression of the disease. Try to find enjoyable activities that are within your physical capabilities.
It is important that family and other people in the patient’s environment are open regarding MS. Relatives too are often overwhelmed by the diagnosis. Talking to each other about the uncertainties and the challenges can prevent misunderstandings.
Every patient develops his or her own strategies when living with MS.
Author: Saskia Wibner
Sources:
Wiendl, H., Korsukewitz, C. & Kieseier, B. (2021). Multiple Sklerose: Klinik, Diagnostik und Therapie. 2. Erweiterte Auflage. Kohlhammer Verlag
Hansen, S., Wettinger, L. & Keune, P. (2021). Multiple Sklerose. Hogrefe Verlag.
Epigenetic aspects of multiple sclerosis and future therapeutic options (2021)
Multiple Sclerosis Epidemiologic, Clinical, and Therapeutic Aspects (2017)
Differential diagnosis of multiple sclerosis and other inflammatory CNS diseases (2019)
Rehabilitation for people with multiple sclerosis: an overview of Cochrane Reviews (2019)
You might also be interested in
4. April 2023
Health
Rehabilitation
Stroke nutrition guidelines for optimal health
Nutrition as the key part in health and well-being of stroke survivors A healthy, balanced …
21. March 2023
Rehabilitation
Kinesio taping in neurology as a useful therapy supplement
The Kinesio tape and its usefulness in neurological therapy What was originally known only from …
7. March 2023
Rehabilitation
Exercises against freezing of gait in Parkinson’s disease
When the legs freeze – how does the symptom “Freezing of Gait” manifest itself? Parkinson’s …



 Contact
Contact 

 Contact
Contact